 |
|
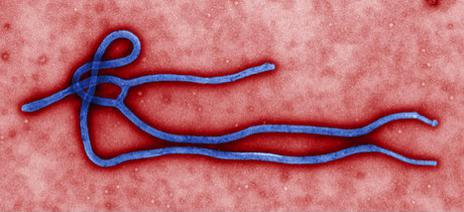
At the time of this article, we are in the midst of the deadliest epidemic of Ebola in history. Thus far, although the World Health Organization believes that the figure is an underestimate, 9216 persons have been infected and 4555 have died, with a mortality of 50%. But amidst the chaotic and panicked conversations, there is a lot of confusion about the disease. How did the virus start in the first place? Why did it originate in Africa? Why is it so deadly? How does it cause deaths? Is it really airborne? What treatment is there? Is mass panic and hysteria warranted at this stage? Are we prepared to handle cases in our island? To be able to provide answers to these as well as other questions, a proper understanding of the disease is required.
Where did Ebola come from?
Ebola is a virus which, evidence suggests, normally lives harmlessly in fruit bats in equatorial forests of Africa. These bats, although carrying the virus within them, are not affected by it and therefore do not normally display any symptoms or die as a result of the virus. Animals that harbor viruses (or bacteria) within them and remain asymptomatic are called hosts. These bats can also drop half eaten fruits which are consumed by other forest animals that are subsequently infected. Human contact with blood, body secretions and fluids from these animals can result in transmission of the virus from the animal to humans.
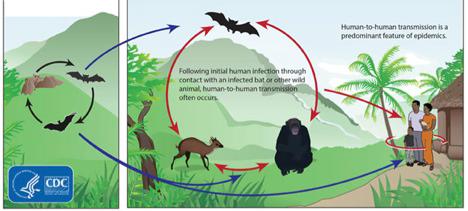
The process of transmission of a virus or bacteria from an asymptomatic animal host to a human is called Zoonosis and is not specific to the transmission of Ebola by bats, since this is also seen in rabies (transmitted to humans from rats and dogs) and certain types of flu (transmitted to humans via birds) among others.
There were two outbreaks of Ebola previously, both in 1976, and they took place in Sudan and Congo which are also African countries. In fact, there is a river in the Democratic Republic of Congo called the Ebola River near the village where the first outbreak started and from which the disease got its name.
Who were the first cases of Ebola in this current epidemic and how were they infected?
The current outbreak started in December 2013 in a village called Meliandou, in southeastern Guinea. The first known case was a two year old boy named Emile who died on December 6th 2013 after having experienced fever, vomiting and diarrhea. It is suspected that he was infected by direct contact with an infected bat since reports suggest that his family hunted bats as meat. His mother, sister and grandmother passed away shortly thereafter with the same symptoms. The disease continued to spread from this point to the surrounding villages, since these were the persons who were taking care of the ill family, as well as to those who had direct contact with the bodies up until the funeral.
How is Ebola transmitted?
Human to human transmission occurs when body fluids (including blood, saliva, vomit, faeces, urine, sweat, breast milk and semen) from an infected person or objects (including clothing, surfaces and medical supplies) contaminated with these fluids (which contain virus particles) come into direct contact with broken skin (a cut or bruise) or an exposed mucous membrane (eyes, nose and mouth) of a previously uninfected human. Of particular significance regarding body fluids is that, in those who survive the disease, they can still transmit the disease to other persons by way of bodily secretions, including semen and breast milk, for an extended period of time. It has been found that men who have recovered from Ebola remain capable of transmitting the virus (which is still persisting within their bodies) for up to 7 weeks in semen.
I have heard some people saying recently that Ebola is now an airborne disease. Is this true?
Simply put, the answer is no. By definition, an airborne disease is one which, on aerosolized dust or liquid, stays suspended in air currents long enough to travel for considerable distances on air currents and causes infection at a distance between the source and the person infected.
Examples of diseases which are spread by airborne mechanisms include influenza, measles, chicken pox, anthrax and tuberculosis.
The Centers for Disease Control and Prevention (CDC) did update their statement on Ebola transmission to include the probability that, although coughing and sneezing are not normally symptoms of Ebola infection, if a symptomatic patient sneezes or coughs (for any reason) and expels saliva or mucus in this way directly onto unprotected mucous membrane surfaces or broken skin of an uninfected person, the viral particles in the secretions can cause infection. There is no evidence currently to suggest that the Ebola viral particles can float independently around in the air and be inhaled to cause infection at a later point in the day.
How is it that three separate countries ended up with Ebola at the same time?
As can be seen from the map outline below, these first cases are located near the border of Guinea, in close proximity to the borders of both Sierra Leone and Liberia. The virus continued spreading person to person and village to village until it spilled over into these two other countries.

Even though the disease started in December 2013, it was only in March 2014 that officials notified the Health Ministry in Guinea that there was an upsurge in an unidentified lethal illness. By the time it was investigated and identified as Ebola, significant human to human transmission had already occurred and the region was well into the epidemic. On August 8th 2014, the World Health Organization’s Director-General declared this outbreak a Public Health Emergency of International Concern.
Why is the Ebola virus more dangerous that other viruses?
In an ordinary viral infection, once the viral particles enter the blood, dendritic cells normally ingest them (having detected them as being potentially harmful), process them and signal an alarm which activates the immune system for other immune system cells to produce antibodies to fight that particular virus. These antibodies then float around in the circulation, hunt down the virus particles and stick on to their surface, preventing them from entering and infecting more cells, and the virus is cleared from the body. This process normally takes a few days and due to this controlled immune response the infected person slowly recovers. The Ebola virus, however, is much more lethal and, at the end, causes your own immune system to attack and kill you.
Once the Ebola virus enters the body, it immediately infects the immune system cells, targeting the dendritic cells. It silently infiltrates the dendritic cells and silences the alarm which is supposed to activate the rest of the immune system. Since there is no resistance from the immune system defences, this results in the virus multiplying at a rate of millions of viral particles per day.
The time interval between the moment the virus enters the body (patient becomes infected) and the development of symptoms is called the incubation period and this varies from 2 to 21 days, with an average interval of 8 to 10 days.
The early symptoms of Ebola are initially similar to the symptoms from any other viral illness:
-
Fever
-
Headache
-
Body pain
-
Weakness
-
Abdominal pain
-
Vomiting
-
Diarrhoea
Once symptoms have started, the patient becomes infectious, that is, he/she is able to transmit the virus to direct contacts in the manner described above.

The virus continues infecting cells, killing cells which make up organs. The dying cells release their chemical and viral contents into the bloodstream as they rupture. This acts as an “SOS” signal to the immune system which is suddenly made aware that it is under severe attack. It responds in extreme manner by activating every possible immune response simultaneously in an “all-out” attack against the virus, a response called the “cytokine storm”. It is this late but desperate response of our immune system to the virus that causes the most problems. Although some viral particles are killed, the blood vessels of the body suffer the greatest collateral damage.
The “cytokine storm” causes the blood vessels to become porous. The arteries, veins and capillaries start to leak blood and plasma, leading to spontaneous bleeding from multiple areas of the body: eyes, ears, mouth, vomit and diarrhea. It also causes the production of nitric oxide which further increases bleeding and dilates the blood vessels, causing a further drop in blood pressure, drop in body temperature and consequently shock, which is unrelated to, but compounded by, the blood loss.
How is Ebola treated?
There is no cure for Ebola, as for many other viruses. Because it progresses and replicates so quickly, comprehensive treatment in a well-equipped medical facility does increase the chances of survival. In West Africa, because resources are severely limited, patients are often sent home to die because there is no more space at the treatment facilities where patients are being housed.
Supportive care is essential.
-
Intravenous fluids are given to replace the fluids patients are losing from vomiting, diarrhea and leaking blood vessels.
-
Ventilators are used to keep oxygen level high in the bloodstream.
-
Blood transfusions to replace blood lost.
-
Medications to keep the blood pressure from dropping too low for the reasons mentioned above.
Essentially, if the infected person can be kept strong enough for a while, and with the medications, be able overcome the initial damage that the immune system does in trying to fight the infection, their immune system might eventually be able to clear the virus on its own. The critical part of the illness is to be able to overcome the cytokine storm which occurs initially. The cost of the care mentioned above required to maximize the chances of survival is approximately 1,000 US dollars per day.
What experimental medications are being given to some of these patients?
Because Ebola is a virus, medications that are approved for use in the management of some other viral illnesses are being given to some of these patients to see if they will help, although they have not been studied for use in Ebola patients. These medications include some HIV medications and immunoglobulins.
Are there any special chemicals that can be used to kill the virus?
Hospital grade-disinfectants (basically household bleaches) are sufficient for sterilizing potentially contaminated surfaces since this has been proven to kill the virus. Of course, the appropriate protective equipment must be worn while doing this decontamination.
How long can Ebola survive outside the body?
On surfaces such as counter tops, doors and trolleys the Ebola virus can survive for a few hours. In contrast, it can survive for many days in body fluids which, if not disposed of properly, can result in direct transmission to an unsuspecting individual.
Which countries have had cases of Ebola?
These can be divided into the following categories:
-
Countries with overwhelming transmission:
a. Guinea
b. Liberia
c. Sierra Leone
-
Countries with transmission within their borders (persons who have been externally infected but after returning to their home country have passed the infection on to others in their home country):
a. Nigeria
b. Spain
c. United States
-
Countries with a single isolated case
a. Senegal
-
Countries treating medically evacuated cases:
a. France (1 case – full recovery)
b. Germany (3 cases – 2 recoveries, 1 death)
c. Norway (1 case – full recovery)
d. Switzerland (monitoring 1 suspected case)
e. United Kingdon (1 case – full recovery)
f. United States
The controversial question some are asking is this: why are foreign nationals who are diagnosed with Ebola flown back to their home (or another country) to receive treatment and risk infecting others and starting an epidemic in their country? This is called repatriation and is essentially because either the patient or his/her employer (or both) desires the best medical care available and is not convinced that this is possible in the country in which he/she was infected. Thus far, there have been about 15 high-risk evacuees. The cost involved in repatriation is significant since a hazmat (hazardous materials suit) team and an airplane are used per single person because no one else can be on the plane during transport. A general cost is in the region of 200,000 US dollars. Typically, the organization that employed the individual (or the organization's insurance company) pays the bill. There have been documented instances where the infected person died awaiting either approval or release of funds for transport.
A high-risk individual should be evacuated in a plane with a biological containment unit. That way, pilots, medical staff and ground crew are kept out of harm's way.

Thus far, all United States nationals who have been infected with Ebola have been repatriated to the US and treated. Most of the media coverage has been centered around following the patients diagnosed with Ebola in the US, but as can be seen above, there are other countries who have either treated or are still treating Ebola patients.
The following table details the updates regarding the cases of Ebola in the US at the time of this article:
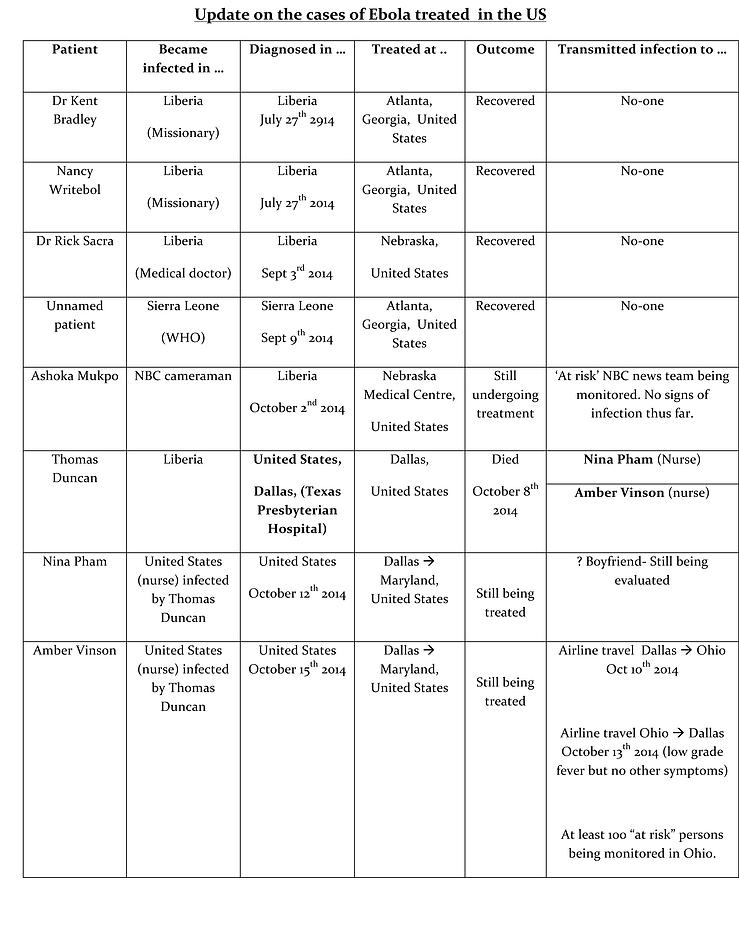
Receiving particular media coverage was the case of Mr. Thomas Duncan who, on September 20th 2014, arrived in the US from Liberia to visit his family. He visited the Texas Presbyterian Hospital in Dallas complaining about fever and disclosed that he had travelled recently from Liberia. He was discharged with antibiotics and Tylenol. (This omission on the part of the hospital has been the topic of much debate and has prompted the issuing an apology from the Hospital administrators). He returned 2 days later via ambulance and was isolated at this time and tested for Ebola. The test returned positive on September 30th, making Duncan the first case of Ebola which was diagnosed on US soil. Duncan died of the virus on October 8th at Texas Presbyterian.
Are there any success stories in the management of the Ebola epidemic?
It is heartening to see that countries with fewer resources than the United States have been able to contain the spread of the Ebola virus. This success story is briefly detailed below so that an appreciation can be gained as to how every country should respond in the event that a case is either suspected or diagnosed within its borders.
On July 8th 2014, one of many patients died of the Ebola virus in Liberia. The patient’s relative, Mr Patrick Sawyer, who was caring for the patient prior to death, was himself hospitalized in Liberia with symptoms of Ebola virus (including fever) but left medical care on July 17th against medical advice. On July 2oth, Mr Sawyer (a Liberian-American development consultant) boarded a commercial plane in Liberia and disembarked in Nigeria. He collapsed in the airport and was transferred to the hospital. At the hospital, he claimed that he had no known exposure to Ebola and this caused the medical staff to initially treat him for malaria, which also has the same symptoms. His medical team became suspicious when he did not respond to malaria treatment and suspected Ebola, given his travel history. He was put into isolation and tests done which confirmed him as being Nigeria’s first Ebola case (index case). He later died of the virus on July 25th 2014.
Once he was diagnosed, Nigeria’s public health response was to immediately identify a total of 989 persons as being “at risk”. The list included everyone who had contact with him when he collapsed in the airport, those who were with him on the aircraft, his attending medical team and their respective direct contacts. This number tallied 351. Unfortunately, he had passed the infection on to another individual while he was ill but prior to being admitted to hospital a second case had transmitted the virus to 3 further persons, among whom included a medical staff member attending to him. This person then generated his own list of 526 “at risk” persons. These totaled 989 persons who were then meticulously tracked down, monitored and evaluated for development of symptoms. Any persons showing any symptoms were immediately transferred to a special treatment center for further evaluation, their contacts recorded and located and decontamination performed. Persons whose tests for Ebola came back negative but still had viral symptoms were monitored separately from those who were confirmed as positive for Ebola. A total of 19 persons developed Ebola out of the 989 patients who were being monitored. The last case was diagnosed on September 8th 2014. After 21 days of full monitoring, no further cases of Ebola have developed in Nigeria and the WHO has declared Nigeria Ebola free after the virus claimed a total of 8 lives, 4 of whom were health care workers and their family members.
Senegal confirmed its first case of Ebola on August 29th 2014 after an infected person entered the country from Guinea. Following diagnosis, 67 “at risk” contacts of the case were identified and monitored. Of these 67 persons, five developed suspicious symptoms and were tested but all test results were negative. The patient who was diagnosed has made a full recovery.
Both Senegal and Nigeria have been declared Ebola-free by the WHO since they have passed the benchmark of surveillance of 21 days (the incubation period of the virus) with no cases being diagnosed.
This tremendous success in stopping the virus from progressing involved three key elements in the response:
(1) The rapid and thorough tracing of all potential contacts.
(2) The ongoing monitoring of all these contacts.
(3) The rapid isolation of potentially infectious contacts.
Are there any cases of Ebola in the Caribbean?
There are currently NO cases of Ebola in the Caribbean. The Caribbean Public Health Agency (CARPHA) director Dr. James Hospedales is working with all Caribbean Health Ministries and local Health Officials to “maintain a high level of preparedness and make sure all measures are in place which meet with the conditions of the international health regulations.”
What is the Health Ministry in Trinidad doing to prevent the virus from reaching our shores?
On the 16th October 2014, the Health Minister, Dr. Fuad Khan announced at a post-cabinet news conference the following precautions:
-
Persons coming to Trinidad from the following countries will be denied entry into Trinidad and Tobago:
-
Sierra Leone
-
Guinea
-
The Democratic Republic of the Congo
-
Liberia
-
Nigeria.
-
(On 22nd October 2014, Health Minister Dr. Khan announced that the ban on travelers from Nigeria had been lifted).
-
Persons who visited the above mentioned African countries within the past six weeks will also not be allowed entry.
-
Citizens who visited these countries will be quarantined for 21 days upon arrival in Trinidad and Tobago.
-
Thermal imaging cameras are being purchased by the Government of Trinidad and Tobago for the purpose of monitoring passengers arriving at both Piarco and Scarborough Airports. Thermal imaging cameras are utilized to identify and measure the amount of heat that objects produce and hence are basically screening for fevers in passengers. Although such a camera cannot be relied upon by itself, it will increase the chances of detection of suspected cases (who may require further medical assessment) when combined with screening cards and oral assessment by immigration officers.
What measures have been put in place if a suspected case of Ebola reaches Trinidad and Tobago shores?
According to Dr Furlonge, a 12-bed area has been set up at the Eric Williams Medical Sciences Complex (EWMSC) Mt Hope, for the purpose of triaging suspected cases. Additionally, two 24-bed wards have also been set up at the Caura Hospital in the event it is necessary to quarantine anyone. Three rooms had also been identified at the EWMSC Intensive Care Unit, which will be capable of providing isolation and ensuring clinical care is to be administered.
Ongoing stakeholder meetings are continuously being held on a local, regional and international level, with Ministries of Health and National Security being at the forefront, but involving many other stakeholders in a bid to maximize readiness capacity if and when the situation arises.
So, where does all of this leave us?
Anxiety has been the order of the day regarding Ebola. No country would ever want to be in a position of having to manage an Ebola epidemic and therefore we must continue to remain vigilant at our ports of entry.
As citizens, knowledge of the Ebola virus and what you can do is just as important since in the unfortunate event that a case reaches our country, personal precautions will be even more crucial. Keep updated and do not panic unnecessarily. Practice good hygiene always. Remember that you must be in direct contact with an infected case to get the Ebola virus. Our best offence is defense.
Given the concern in the national (and international) community about Ebola, I will attempt to provide answers to as many questions as possible which are posted in the comments section below.
The information provided in this column is for general educational purposes only and is not meant to provide professional assistance nor is it intended to diagnose or treat any condition. If you are dealing with a serious medical problem, you are strongly advised to schedule an appointment and visit with a qualified medical practitioner. While every effort has been made to make the contents of this column as up to date as possible, it should be noted that statistics and guidelines for Ebola change regularly.
| By: Dr. Joseph Ramdhanie | FEATURES | November 2014 |
Tweet |
Warning: array_search() expects parameter 2 to be array, null given in /home/paradisepulsea/public_html/pages/article.php on line 87
Warning: in_array() expects parameter 2 to be array, null given in /home/paradisepulsea/public_html/pages/article.php on line 104
Warning: array_search() expects parameter 2 to be array, null given in /home/paradisepulsea/public_html/pages/article.php on line 87
Warning: in_array() expects parameter 2 to be array, null given in /home/paradisepulsea/public_html/pages/article.php on line 104
Warning: array_search() expects parameter 2 to be array, null given in /home/paradisepulsea/public_html/pages/article.php on line 87
Warning: in_array() expects parameter 2 to be array, null given in /home/paradisepulsea/public_html/pages/article.php on line 104


| Subscribe |